The benefits of integrating pharmacy & medical assistants

In today’s fast-changing healthcare climate, integrated healthcare roles are an important way to provide quality, patient-centered care. By integrating pharmacy and medical assistant roles, including pharmacists and pharmacy technicians, facilities can develop a cohesive, effective interdisciplinary healthcare team, which improves patient outcomes and enhances the goal of increased healthcare efficiency in diverse care settings.
This blog will provide insight into how combining these roles can create greater continuity in care, reduce the chance of errors, and promote a sense of shared accountability. Ultimately, the embrace of integrated healthcare roles is a great initiative for any facility to undertake to stay ahead of the curve in a rapidly changing healthcare environment.
How healthcare roles overlap and complement each other
Integrating pharmacy team members—such as pharmacy technicians or pharmacists,with staff through integrated healthcare roles enhances care quality and coordination. To support this model effectively, it is important to hire medical assistants who can contribute to team-based care. This collaboration strengthens efforts in medication management and patient education, helping reduce errors and improve outcomes.
Each role plays a distinct yet complementary part: pharmacists take the lead on clinical decision-making, verifying prescriptions, and managing complex medication therapies. Pharmacy technicians handle logistical tasks such as medication preparation, inventory, and administrative documentation. Meanwhile, medical assistants act as the frontline connectors, facilitating communication, scheduling, and reinforcing medication instructions with patients. When all three roles are aligned, the patient experience becomes more seamless and safer.
To ensure these roles function effectively, it is essential to hire pharmacy technicians or pharmacists, and medical assistants who are well-qualified and capable of supporting interdisciplinary teamwork. Strategic hiring practices play a key role in building a team that can deliver consistent, patient-centered support across various care settings.
Also read:
Strategies to hire medical assistants and retain them
The advantages of the team-based approach include:
- Streamlined workflows and reduced duplication of tasks: When pharmacists, pharmacy technicians, and medical assistants understand each other’s responsibilities, it eliminates repetitive work and allows the team to focus on critical care tasks, boosting overall efficiency.
- Faster identification and resolution of care gaps: Interdisciplinary collaboration helps flag issues early—such as missed doses or patient non-compliance—enabling proactive interventions that improve treatment outcomes.
- Increased patient satisfaction and trust: Patients benefit from consistent communication and coordinated care, which builds confidence in their providers and leads to higher satisfaction scores and improved retention.
The role of communication in interdisciplinary healthcare teams
Good communication is the cornerstone of interdisciplinary healthcare roles. Having routine updates, shared digital records, and well-defined protocols in place means that every member of the team is aligned.
Seamless communication is necessary for enhancing healthcare efficiency and for the efficient functioning of an interdisciplinary healthcare team. Along with tools and processes, communication and soft skills like listening, speaking clearly, and being respectful help teams work better together, which is why a healthcare facility needs to hire pharmacists, pharmacy technicians, and medical assistants who bring both clinical expertise and strong interpersonal skills.
Also read: The value of soft skills in hiring pharmacy techs & NPs
Examples of how communication can be applied:
- Weekly huddles with pharmacy personnel and medical assistants to review patient cases
- Electronic health records (EHRs) are used to communicate medication updates and patient notes
- Medication reconciliation and patient education checklists
The growing adoption of electronic health records (EHRs) has played a major role in improving interdisciplinary coordination, as further illustrated in the table below.
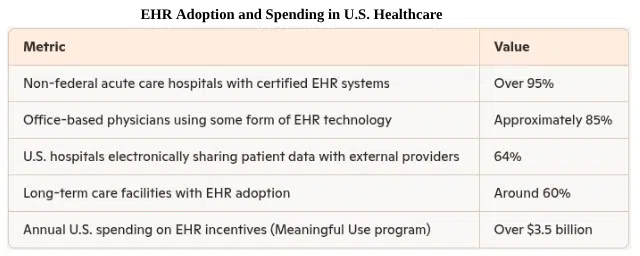
Source: https://media.market.us
Addressing common barriers in integrated healthcare roles
Integrating pharmacy and medical assistant roles brings many benefits, but it also presents challenges. Differences in workflow, compliance requirements, and building mutual trust can create barriers. These obstacles often emerge when pharmacists, pharmacy technicians, and medical assistants begin working in shared care models without clear coordination. Differences in role expectations, variations in clinical training, and unclear communication channels can lead to confusion or duplicated efforts.
For example, if medication updates are not documented, both the pharmacist and medical assistant may assume someone else has followed up, delaying patient care.
In some cases, team members may feel undervalued if their role is not fully understood by others. These issues can disrupt the workflow and impact healthcare efficiency, especially in high-volume settings. Addressing them early through structured collaboration can significantly reduce friction and build a more unified care environment.
Successful integration relies on defining each role’s contribution. Pharmacists manage clinical oversight and safety checks; pharmacy technicians support preparation, inventory, and technical workflows; and medical assistants help bridge communication between the care team and patients. When integrated properly, these roles reduce redundancies and ensure a smooth, team-based approach to patient care.
However, with clear leadership and continuous training, these challenges can be overcome, strengthening the interdisciplinary healthcare team and supporting integrated healthcare roles.
Common challenges and solutions:
- Workflow alignment: Implement cross-training sessions to familiarize both roles with each other’s responsibilities
- Compliance: Develop shared protocols for documentation and patient privacy
- Trust-building: Encourage open and positive feedback and recognize team achievements
Real-world results and practical action steps
Facilities that have adopted integrated healthcare roles and concentrated on integrating pharmacy and medical assistant functions report remarkable improvement in patient outcomes and a productivity boost. With more facilities recognizing its long-term value, the real-time example model is steadily becoming a standard in progressive healthcare systems.
Actionable steps to be followed:
- Evaluate existing team compositions and determine the potential for greater integration
- Invest in shared training programs for medical assistants and pharmacy staff
- Employ current technology to automate communication and documentation
Several healthcare facilities have implemented comprehensive transitional care programs involving multiple healthcare roles and have achieved improved outcomes—one such example is outlined below.
For instance, Kaiser Permanente Southern California implemented a comprehensive transitional care program—including medication reconciliation, post-discharge follow-up, and risk stratification—which led to noticeable improvements in patient outcomes and reduced hospital readmissions across several medical centers. This real-world initiative highlights how structured collaboration between clinical roles can make a meaningful difference in care quality.
The key elements and results of this program are summarized in the infographic below for easier understanding.
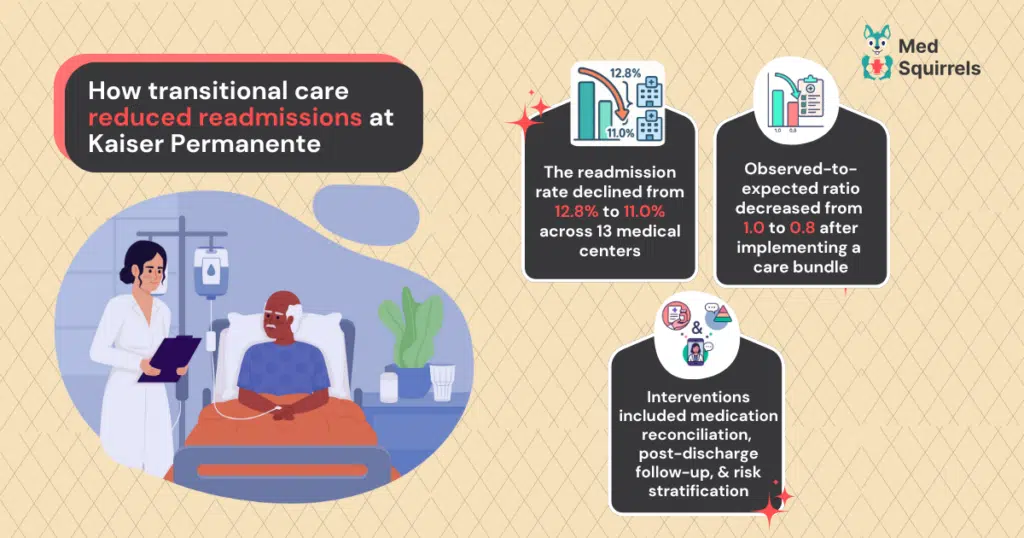
These favorable results highlight the importance of a coordinated interprofessional healthcare team in enhancing efficiency. By placing integrated healthcare roles and collaboration at the top of the agenda, healthcare organizations can provide safer, more effective, and more efficient patient care
Modern staffing for integrated roles with MedSquirrels
In today’s fast-moving healthcare world, partnering with a reliable healthcare staffing agency is key to building strong, integrated healthcare roles and improving team-based care. While traditional agencies have assisted in the past, many healthcare facilities now face issues like slow hiring and high placement costs, which can hold back patient services and stretch budgets.
To avoid these staffing problems, more healthcare facilities are choosing modern platforms like MedSquirrels a tech-powered healthcare staffing platform that offers faster and more affordable staffing services.
Unlike traditional methods, MedSquirrels connects you directly with qualified professionals and uses smart AI technology to streamline recruitment, onboarding, and compliance for integrating pharmacy and medical assistant roles.
Its affordable, flat-fee plans are made for every type of facility:
Orange Plan – A full-service solution covering recruitment, credentialing, onboarding, and EOR/payrolling for contract or full-time staff. This Orange Plan is ideal for facilities looking to outsource the entire hiring process with minimal internal effort.
Purple Plan – Best suited if you have already selected a candidate and need seamless EOR/payrolling support to ensure compliance, timely payments, and reduced administrative workload.
Blue Plan – Focused on recruitment-only support for full-time hires, perfect for filling long-term clinical roles efficiently with access to a vetted talent pool and quicker time-to-hire.
These cost-effective plans are designed for clinics, hospitals, or multi-site healthcare facilities, supporting interdisciplinary healthcare teams and enhancing healthcare efficiency. With no hidden fees, faster hiring, and complete transparency, MedSquirrels makes it easier to build a strong, integrated team. Ready to streamline your healthcare hiring process? Click here to book a free demo.
FAQs
What are integrated healthcare roles, and why are they important?
Integrated healthcare roles involve collaboration across disciplines—like pharmacy and medical assistants—to improve care coordination, patient outcomes, and team efficiency. These roles reduce duplication of effort and promote more holistic, patient-centered care.
How do interdisciplinary healthcare teams improve care delivery?
Interdisciplinary teams bring together varied expertise to assess, treat, and follow up with patients more effectively. By working collaboratively, these teams reduce communication errors and ensure no aspect of patient care is overlooked.
What is medication reconciliation, and how does it relate to role integration?
Medication reconciliation is the process of ensuring a patient’s medication list is accurate and complete at transitions of care. When pharmacy and medical assistant roles are integrated, they can coordinate on this task to reduce errors and improve patient safety.
Does MedSquirrels support compliance and credentialing?
Yes. MedSquirrels supports facilities by helping ensure candidates meet credentialing and compliance requirements throughout the hiring and onboarding process. This helps healthcare providers stay aligned with industry regulations.
Is MedSquirrels suitable for small clinics or only for large hospital systems?
Yes, MedSquirrels is built to support healthcare facilities of all sizes. Whether you’re managing a small outpatient clinic or a multi-site system, the platform’s flexible, cost-effective plans make it easy to scale hiring as needed.
Jani Basha is a healthcare content expert at MedSquirrels, sharing insights on staffing trends, hiring best practices, and career growth.
