How credentialing delays impact patient care and revenue
In the healthcare industry, validating a provider’s credentials—a process known as provider credentialing—is required prior to treating patients or billing for services. But the process too often takes far too long. Slow credentialing not only holds up documents, but it also leads to staff burnout, patient care delays, and significant revenue losses.
This blog describes why slow credentialing occurs, what issues it creates for healthcare staff, and how facilities can correct it. You will discover the true costs of these delays and real-world solutions to enhance medical credentialing so your staff remains productive, patients receive care on time, and your revenue remains on track.
Whether you operate a large hospital or a small clinic, it is essential to know these challenges to enhance operations. With the proper approach, healthcare credentialing can be an asset, not an obstacle.
Understanding credentialing and its challenges
Credentialing is the validation process that ensures healthcare professionals are qualified and competent to practice. It includes license verification, background checks, malpractice history, and more. Despite being essential, it is often plagued by inefficiencies and outdated methods. Many facilities still rely on manual systems that are vulnerable to errors and delays.
These outdated approaches not only slow down onboarding but also increase the likelihood of regulatory risks and operational disruptions. Inefficient processes and a lack of standardization play a significant role in causing delays and administrative barriers. Poor healthcare facilities and incomplete documentation are common causes of inefficient credentialing, resulting in missed deadlines and compliance problems.
The ripple effects of slow credentialing
When credentialing deadlines are slow, the effects ripple. Staff are buried under work, providers sit idle, and healthcare facilities lose revenue. Burned-out HR and credentialing staff are frequently a result, with retention next to impossible. Patients are eventually affected through increased wait times and restricted provider access. This creates a cycle where provider shortages worsen, and overburdened staff are left to manage growing demands with limited resources.
- Slow credentialing is a heavy burden on HR teams, escalating burnout and decreasing morale with manual follow-up and backlogs.
- Delays in onboarding new providers diminish access to care, decrease patient satisfaction, and create significant gaps in services. These issues eat up resources and result in lost opportunities. Staffing errors can significantly contribute to inefficiencies.
Check out: The hidden costs of poor healthcare staffing decisions.
The true cost of slow credentialing in healthcare
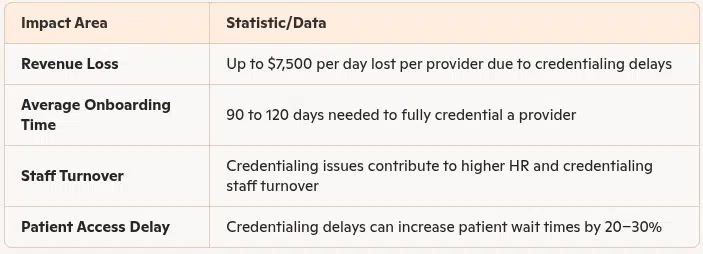
Source: www.beckershospitalreview.com
Solutions to streamline credentialing
Effective medical credentialing demands an active, technology-enhanced, workflow-transparent, and trained staff-based approach. Standard checklists and automation can eliminate common errors and minimize wasted time. Healthcare facilities must review existing systems and update them as necessary to respond to current demands.
By addressing workflow inefficiencies and unifying communication among departments, facilities can significantly reduce delays and improve compliance.
- Employ automated solutions and databases to reduce unnecessary credentialing and repetitive steps in the credentialing cycle.
- Integrate a detailed nurse credentialing checklist, which includes vital steps like verifying licenses, certifications, background checks, and standardized practices that initiate consistent procedures for documenting, reviewing, and verifying credentials to ensure completeness and accuracy of all documentation.
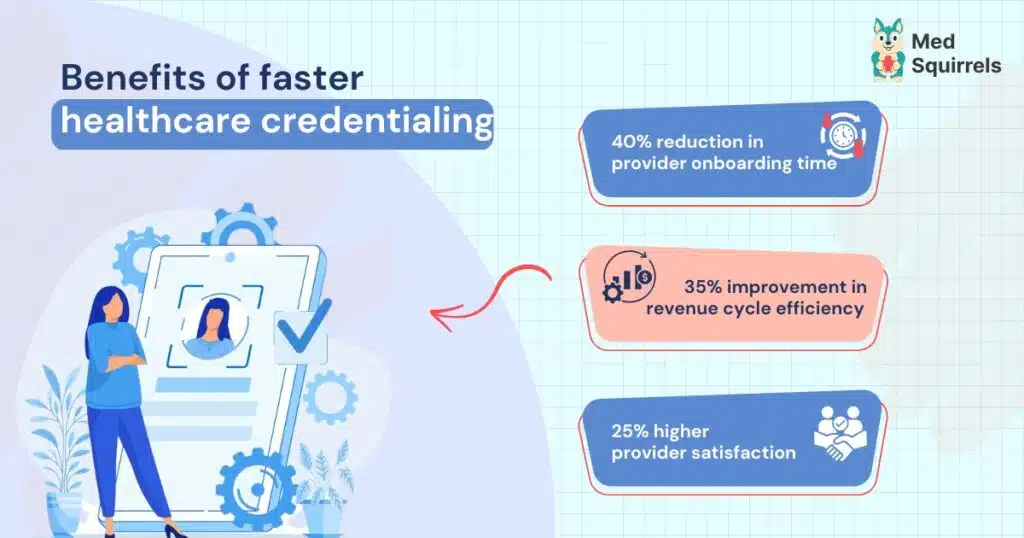
The financial and operational benefits of faster credentialing
Streamlining provider credentialing is not only compliance—it serves immediate operational objectives, revenue growth, and patient satisfaction. Providers who are credentialed can start seeing patients and billing sooner. It also minimizes the burden on other employees, which enhances morale and decreases turnover. Facilities that automate credentialing have a competitive advantage and can grow more rapidly. In fact, reducing bottlenecks in credentialing is one of the quickest ways to improve financial health and care delivery efficiency across your facility. Faster turnaround times cut down on staffing shortages, enabling new providers to bring in revenue sooner and reducing scheduling disruptions. A robust credentialing system enhances retention and provider satisfaction by preventing provider credentialing errors that usually infuriate new hires.
Read more: Why facilities prefer staffing platforms for quick credentialing and onboarding.
Overcoming slow credentialing challenges with MedSquirrels
Slow credentialing impacts the entire function of a healthcare facility. It slows down patient care, results in a loss of revenue, and causes difficulties for employees and management. Conventional staffing sites tend to use outdated practices that slow down the process of hiring, waste precious time, and cause financial pressure. These challenges drain resources and lead to missed opportunities.
MedSquirrels exists to fix these issues, its staffing platform form facilitates healthcare credentialing to be quicker and easier. Through streamlining, it reduces paperwork, minimizes provider credentialing errors, and expedites onboarding. It results in new providers being able to see patients sooner, which directly impacts your healthcare facility. Partnering with MedSquirrels can help your facility avoid the issues caused by slow credentialing. The platform offers a smooth, automated process that saves time and ensures accuracy.
Faster onboarding means your team can meet patient demand more effectively, and the smoother your operations run, the better the patient care you can provide. With MedSquirrels, your facility can boost productivity by a swift credentialing process and speeding up provider onboarding. This helps your team focus more on patient care, reduce delays, and improve patient outcomes.
To help your facility achieve these benefits, MedSquirrels offers three cost-effective plans designed to meet the needs of your facility and streamline your credentialing process even further. Each plan is created to simplify and optimize your workflow, allowing you to focus more on patient care and operational efficiency. Here is a breakdown of the plans available to you:
- Orange Plan: This plan combines recruitment and payrolling services. MedSquirrels handles recruitment, onboarding, credentialing, benefits, and compliance for both contract and full-time staff. Includes an employer-of-record (EOR) service for hassle-free management.
- Purple Plan: For those healthcare facilities that have already sourced the right talent, MedSquirrels takes care of payroll, benefits, compliance, and onboarding while eliminating employer obligations, with a focus on contract staff.
- Blue Plan: This plan focuses purely on recruitment. MedSquirrels assists in finding the right professionals suitable for your healthcare facility, handling screening, and interviews. It also offers advice/negotiations.
These three affordable plans streamline the credentialing process by eliminating middlemen and keeping your team well-informed through enhanced email reminders. This improves efficiency, reduces delays, and ensures smoother workflow management. Have questions about how our platform works? Schedule a free demo where we will show you the capabilities of our staffing platform.
FAQs
What is provider credentialing, and why is it important?
Provider credentialing is the process of verifying the qualifications, licenses, and background of healthcare professionals before they can treat patients or bill for services. It ensures that providers meet established standards of care and protect patient safety.
How does slow credentialing impact healthcare facilities?
Slow credentialing can delay patient care, contribute to staff burnout, and cause significant revenue losses by preventing providers from billing for services.
What are the main causes of slow credentialing?
The primary causes include outdated manual processes, incomplete documentation, inefficient communication between departments, and a lack of standardized procedures in healthcare credentialing
How does MedSquirrels solve the problems of slow credentialing?
MedSquirrels helps healthcare facilities avoid credentialing delays by connecting them with qualified, pre-verified providers. By streamlining provider matching and improving communication throughout the credentialing process, MedSquirrels supports faster onboarding, reduces administrative strain, and helps facilities maintain better staffing without disrupting their existing credentialing workflows.
Is MedSquirrels suitable for both small clinics and large hospitals?
Absolutely. Whether you run a small clinic or a major healthcare facility, MedSquirrels is a staffing platform designed to assist your facility according to your credentialing needs and operational size.
Jani Basha is a healthcare content expert at MedSquirrels, sharing insights on staffing trends, hiring best practices, and career growth.
